September is World Alzheimer’s Month; it is a time to raise awareness about Alzheimer’s disease, promote brain health, and support those affected by the condition.
As part of my education to become a Personal Trainer, I had to learn about working with “special populations;” this can refer to youth, those with chronic diseases, and those with disabilities. After my certification as a trainer, I studied to become a Functional Aging Specialist. After obtaining that specialization, I was better prepared to work with older adults living with a wide variety of physical and cognitive conditions. I thought I knew all that I needed to know to work with people living with dementia.
Book-learning and seminars, however, are no substitute for hands-on experience. Over the last seven years, I have had the opportunity to work with several clients at various stages of Alzheimer’s Disease or other forms of cognitive decline. It is interesting and challenging work, and I have learned a lot.
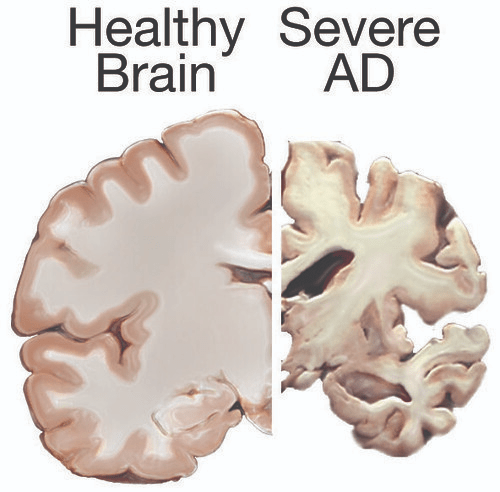
There is a question, though, about what the benefit of such an exercise program might be. I have posted about this in the past, but it bears repeating as we work our way through World Alzheimer’s Month. The only non-medical way in which brain health can be improved is through exercise in conjunction with a proper diet and sufficient rest. The heart pumps and circulates nutrient rich blood to all parts of the body; when we exercise (especially cardio) that process speeds up and brings more nourishment to the cells, including those in the brain. Research shows that regular exercise can help to slow the progression of the disease.
There is another aspect though which should not be overlooked. For some of my clients with dementia, the time that I spend with them is an opportunity to engage socially with someone aside from family or caregivers. I always come prepared for a workout especially designed for the client and his/her capabilities; in that respect, they are no different than my other clients. What is different is the way the session may proceed. I usually need to demonstrate exercises several times–even after we just completed a set; this requires patience on my part, but I have gotten accustomed to this and it has changed the way that I cue all my clients for the better.
Related to this is that I must modulate the conversation that I have with my clients with dementia. Ask any of my clients and they will tell you that I love to chat during our sessions; it helps to engage the client and make the session appear to move more quickly–while still getting the same amount of work done. The kinds of questions I may ask clients with Alzheimer’s Disease and the topics we might discuss are different. In most cases, I cannot ask “how was your weekend?” as they may not remember. I can usually ask about things that happened many years ago (those memories are often preserved), but most of the time I focus on the present moment. I may talk about what is going on in my life or the weather or the local sports teams. I like to focus on the present moment and making the most out of it for my client–from an exercise and social standpoint.
World Alzheimer’s Month is a time to reflect on the way that this disease has affected so many individuals and families. It is a time to advocate for more research (rather than cuts in funding). It is also a month in which we can reach out to those around us with dementia and help to make their present moment just a little bit brighter. I am proud of my role as Personal Trainer in helping to make that a reality.


